Antibiotics have revolutionized the treatment of infectious diseases globally and contributed to the increased life expectancy in the 20th century. However, there is another aspect of antibiotics, which is their negative impact on gut microbiota. The following article discusses the role of microbiota and how antibiotics negatively impact gut microbiota and the overall health of the human body.
What is the role of gut microbiota?
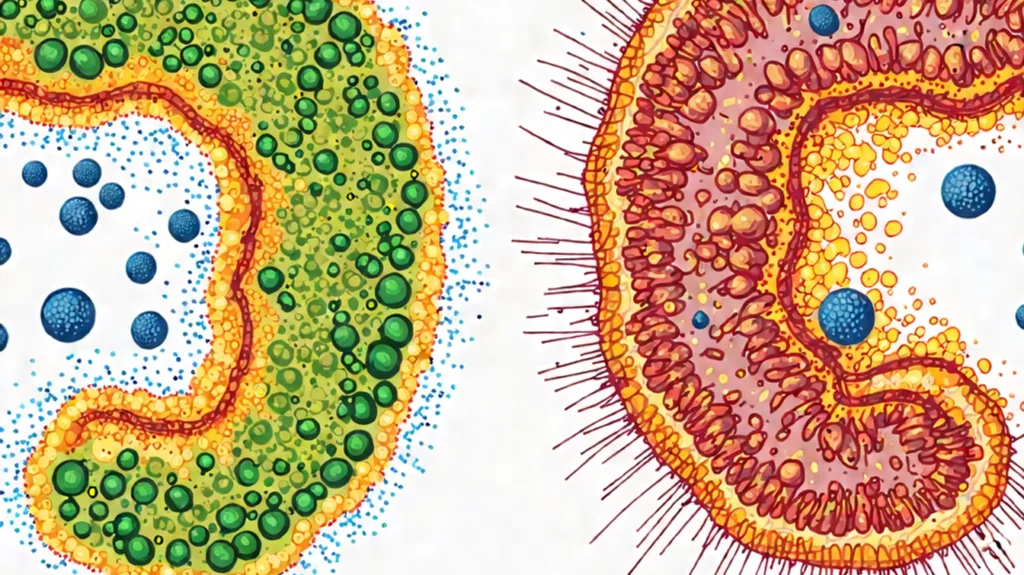
The human gut harbors a complex community of microorganisms, including bacteria, viruses, fungi, and protozoa, collectively known as the gut microbiota. This ecosystem plays a pivotal role in various physiological processes, such as digestion, metabolism, and the modulation of the immune system. A balanced gut microbiota is essential for maintaining health, while disruptions can lead to various diseases. Besides, they are involved in energy homeostasis.
When it comes to babies, the gut microbiota develops during birth. Infant gut microbiota is essential for the development of infant gut immunity. However, it is important to have a balanced microbiota with rich species diversity. Reduced species diversity in an infant’s gut is associated with intestinal illnesses and a predisposition to certain diseases later in life.
Antibiotics and Gut Microbiota
Antibiotics are designed to eliminate pathogenic bacteria, but their broad-spectrum nature often leads to collateral damage, affecting beneficial microbial populations within the gut. This disruption can result in several consequences:
- Reduced Microbial Diversity: Antibiotic treatment can lead to a significant decrease in the richness and diversity of the intestinal microbiota. Studies have shown that treatment with certain antibiotics reduces the richness and diversity of the intestinal microbiota in mice.
- Selection of Antibiotic-Resistant Organisms: The use of antibiotics can drive the generation and spread of antibiotic-resistance genes in gut microbiota. Under selective pressure by antibiotics, sensitive strains are eliminated, giving antibiotic-resistant strains a growth advantage.
- Altered Metabolic Activity: Changes in the composition of the gut microbiota can affect various functions, including immune regulation and metabolic activities, thus impacting overall health.
Consequences of Gut Microbiota Disruption
The disturbances in gut microbiota caused by antibiotics can have several health implications:
- Antibiotic-associated diarrhoea (AAD): Disruption of the gut microbiota can lead to diarrhoea, a common side effect of antibiotic use. This occurs because altering the numbers and species of gut microbiota can reduce the body’s ability to ferment carbohydrates and metabolize bile acids, leading to diarrhoea.
- Clostridioides difficile Infections (CDI): A reduction in levels of native bacterial species disrupts their ability to inhibit the growth of harmful species such as Clostridioides difficile, leading to overgrowth and infection.
- Long-Term Health Effects: Early childhood exposure to antibiotics has been linked to several gastrointestinal, immunologic, and neurocognitive conditions. For instance, studies have suggested that early-life antibiotic exposure may be associated with an increased risk of developing conditions such as asthma, obesity, and attention-deficit/hyperactivity disorder (ADHD).
Antibiotics and Immune System Modulation
The gut microbiota plays a crucial role in the development and function of the immune system. Disruption of this microbial community by antibiotics can lead to:
- Altered Immune Responses: Antibiotic-induced changes in the gut microbiota can affect immune regulation, potentially leading to altered immune responses.
- Increased Susceptibility to Infections: Disruption of the gut microbiota can impair the body’s natural defense mechanisms, potentially increasing susceptibility to infections.
Mitigating the Adverse Effects of Antibiotics
To minimize the negative impact of antibiotics on gut microbiota and immunity, several strategies can be considered:
- Judicious Use of Antibiotics: These drugs should be prescribed only when necessary and with appropriate selection to target specific pathogens, thereby reducing collateral damage to the gut microbiota.
- Probiotic Supplementation: Taking probiotics during and after antibiotic treatment may help restore gut microbial balance. However, it’s important to note that while probiotics can help prevent antibiotic-associated diarrhoea, they may delay the natural recovery of the gut microbiota. Therefore, the use of probiotics should be considered on a case-by-case basis.
- Dietary Interventions: Consuming a diet rich in fiber and fermented foods can support the growth of beneficial gut bacteria, aiding in the restoration of microbial diversity post-antibiotic treatment.
Conclusion
While antibiotics are indispensable tools in modern medicine, their impact on the gut microbiota and immune system is profound. Understanding these effects is crucial for developing strategies to mitigate potential adverse outcomes. By promoting responsible antibiotic use and supporting gut health through diet and lifestyle, we can harness the benefits of antibiotics while minimizing their drawbacks.