Gestational diabetes is a type of diabetes that only happens during pregnancy. It can be a bit scary, but understanding what it is and how to manage it can help you have a healthy pregnancy. This article will explain what gestational diabetes is, what causes it, and what you can do if you have it.
Key Takeaways
- Gestational diabetes is a type of diabetes that only occurs during pregnancy.
- Hormonal changes during pregnancy can make it hard for the body to use insulin properly.
- Being overweight or having a family history of diabetes can increase the risk of developing gestational diabetes.
- Common symptoms include feeling very thirsty, tired, and needing to urinate more often.
- Managing gestational diabetes often involves changes in diet and exercise, and sometimes medication.
Understanding Gestational Diabetes
Definition and Overview
Gestational diabetes mellitus (GDM) is a type of diabetes that occurs only during pregnancy. It affects how your cells use sugar (glucose), leading to high blood sugar levels that can affect your pregnancy and your baby’s health. The condition is usually diagnosed during the second or third trimester and often goes away after the baby is born.
Role of Insulin in Pregnancy
Insulin is a hormone that helps your body convert glucose into energy. During pregnancy, the placenta generates hormones that can increase the resistance of your cells to insulin. This is called insulin resistance. To keep your blood sugar levels normal, your pancreas needs to produce more insulin. If it can’t keep up, your blood sugar levels rise, leading to gestational diabetes.
Impact of the Placenta
The placenta is a temporary organ that forms in the uterus during pregnancy. It is responsible for supplying oxygen and nutrients to the developing fetus while also eliminating waste from the baby’s bloodstream. Additionally, the placenta secretes hormones that can interfere with the mother’s insulin function, leading to insulin resistance. As the placenta expands, it releases a greater quantity of these hormones, which raises the likelihood of gestational diabetes.
Risk Factors for Gestational Diabetes
Age and Ethnicity
Women over the age of 25 are at a higher risk of developing gestational diabetes. Additionally, certain ethnic groups, such as African-American, Hispanic, American Indian, and Asian American, are more likely to develop the condition. It’s important to note that about half of the increased risk may be explained by patients with pre-pregnancy BMI, weight gain during pregnancy, smoking, and illegal drug use.
Other Factors
- Gestational diabetes risk factors in first trimester include having prediabetes or polycystic ovary syndrome (PCOS).
- Having gestational diabetes in a prior pregnancy.
- Delivering a baby who weighed over 9 pounds.
- Being physically inactive.
Understanding these risk factors can help you and your healthcare provider take steps to manage or even prevent gestational diabetes.
Symptoms and Diagnosis
Common Symptoms
Gestational diabetes often doesn’t show clear signs. However, some women may experience:
- Frequent urination
- Excessive thirst
- Fatigue
- Nausea
Other symptoms may include blurry vision, nausea, and vomiting. However, these symptoms might also be common changes associated with pregnancy. That’s why it’s important to get tested.
Screening Tests
To diagnose gestational diabetes, doctors use two main tests:
- Glucose Challenge Test (GCT): You drink a sugary liquid, and your blood sugar is checked after an hour. If your levels are high, you may need a second test.
- Glucose Tolerance Test (GTT): This test is done if the GCT results are high. You will fast overnight and then consume a sugary beverage. Your blood sugar is checked several times over a few hours.
When to Get Tested
Testing usually happens between the 24th and 28th weeks of pregnancy. If you have risk factors like a family history of diabetes or obesity, your doctor might test you earlier. Early detection is key to managing gestational diabetes effectively and ensuring a healthy pregnancy for both mother and baby.
Causes of Gestational Diabetes
Hormonal changes
During pregnancy, the placenta produces hormones that help the baby grow. However, some of these hormones can interfere with the body’s ability to use insulin effectively. This is known as insulin resistance. As the pregnancy progresses, the placenta grows and releases more of these hormones, making it even harder for the body to use insulin.
Insulin Resistance
Insulin is a hormone that helps move glucose from the bloodstream into the cells for energy. When the body becomes resistant to insulin, it needs more insulin to keep blood sugar levels normal. During pregnancy, the pancreas has to work extra hard to produce this additional insulin. If it can’t keep up, blood sugar levels rise, leading to gestational diabetes.
Role of the Pancreas
The pancreas plays a crucial role in managing blood sugar levels. In a healthy pregnancy, the pancreas produces enough insulin to overcome the insulin resistance caused by pregnancy hormones. However, if the pancreas can’t produce enough insulin, blood sugar levels increase, resulting in gestational diabetes.
Understanding what causes gestational diabetes in pregnancy can help in managing and preventing the condition effectively.
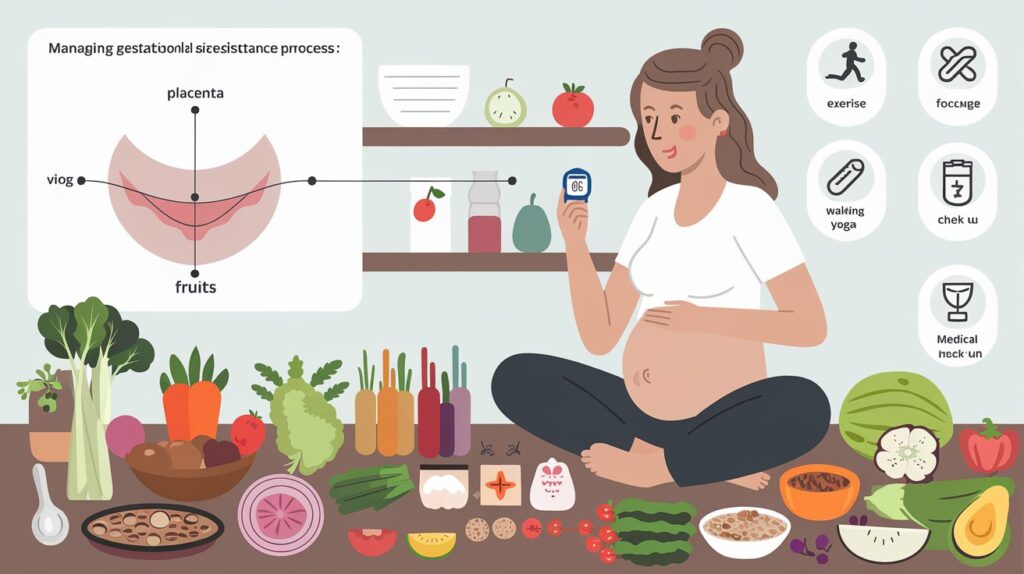
Managing Gestational Diabetes
Dietary Changes
A balanced diet is crucial for managing gestational diabetes. Your doctor can help you develop a meal plan that includes the right mix of nutrients. Here are some general guidelines:
- Eat five servings of vegetables and fruits daily.
- Choose whole grains over refined grains.
- Opt for lean meats and low-fat or nonfat dairy products.
- Use liquid fats like olive oil instead of solid fats like butter.
- Avoid high-calorie snacks and sugary desserts.
Exercise Recommendations
Regular physical activity is another key component. Exercise improves your body’s ability to use insulin more efficiently. Always consult your doctor to determine a safe level of activity for you and your baby. Some safe options include:
- Walking
- Swimming
- Prenatal yoga
Medical Treatments
If lifestyle changes are not enough to control your blood sugar levels, you may need medical treatments. This can include daily blood glucose testing and insulin injections. Your healthcare provider will guide you on how to monitor your blood sugar levels and administer insulin if needed. The goal is to keep your blood glucose levels within the following targets:
| Time | Target Blood Glucose Level |
| Before a meal | 95 mg/dL or less |
| One hour after a meal | 140 mg/dL or less |
| Two hours after a meal | 120 mg/dL or less |
Remember, gestational diabetes is treatable. Working closely with your healthcare team can help ensure a healthy pregnancy.
Potential Complications

For the Mother
Gestational diabetes can lead to several complications for the mother. High blood pressure and preeclampsia are common issues. Preeclampsia is a serious condition that can threaten both the mother and baby’s lives. Additionally, mothers with gestational diabetes are more likely to need a C-section if the fetus gets too big. There’s also a higher risk of developing type 2 diabetes later in life.
For the Baby
Babies born to mothers with gestational diabetes face their own set of risks. They may have an increased birth weight, which can make delivery difficult and may require a C-section. These babies are also at risk for low blood sugar (hypoglycemia) shortly after birth, which can lead to seizures if not treated promptly. Other risks include early (preterm) birth, serious breathing difficulties, and a higher chance of developing obesity and type 2 diabetes later in life.
Long-Term Risks
Both the mother and baby face long-term risks if gestational diabetes is not managed properly. For the mother, there’s a higher chance of developing type 2 diabetes in the future. For the baby, the risks include obesity and type 2 diabetes as they grow older. Careful control of blood sugar levels during pregnancy is crucial to minimize these risks. Managing blood sugar levels carefully during pregnancy can help prevent many of these complications.
Preventive Measures
Healthy Pre-Pregnancy Weight
Starting your pregnancy at a healthy weight can make a big difference. If you’re planning to get pregnant, try to lose any extra weight beforehand. Focus on making lasting changes to your eating habits, like eating more vegetables and fruits. Gaining too much weight too quickly during pregnancy can increase your risk of gestational diabetes. Ask your healthcare provider what a reasonable amount of weight gain is for you.
Regular Physical Activity
Staying active before and during pregnancy can help protect you from developing gestational diabetes. Try to engage in 30 minutes of moderate exercise on most days of the week. Here are some simple ways to stay active:
- Take a brisk daily walk
- Ride your bike
- Swim laps
- Park further away from the store when you run errands
- Take short walk breaks
Early Screening
Early screening can help catch gestational diabetes before it becomes a bigger problem. If you’ve had gestational diabetes before, these healthy choices may also reduce your risk of having it again in future pregnancies or developing type 2 diabetes in the future. Talk to your healthcare provider about when to get tested and what steps you can take to stay healthy.
Conclusion
Gestational diabetes is a condition that can develop during pregnancy, making it harder for the body to use insulin effectively. This can lead to high blood sugar levels, which can affect both the mother and the baby. While the exact cause is not fully understood, factors such as being overweight, having a family history of diabetes, and certain ethnic backgrounds can increase the risk.
The good news is that with early detection and proper management, including diet changes and possibly medication, most women with gestational diabetes can have healthy pregnancies and babies. It’s important to work closely with healthcare providers to monitor and control blood sugar levels. Remember, gestational diabetes is a temporary condition, and with the right care, you can navigate it successfully.
Frequently Asked Questions
Q. What is gestational diabetes?
A. Gestational diabetes is a form of diabetes that develops specifically during pregnancy. It happens when your body can’t make enough insulin to keep your blood sugar levels normal.
Q. What causes gestational diabetes?
A. The exact cause isn’t known, but it is believed that hormones from the placenta can make it harder for your body to use insulin, leading to higher blood sugar levels.
Q. Who is at risk for gestational diabetes?
A. You may be at higher risk if you were overweight before pregnancy, have a family history of diabetes, are over 25 years old, or are of certain ethnic backgrounds like African-American, Hispanic, or Asian.
Q. What are the symptoms of gestational diabetes?
A. Many women don’t have noticeable symptoms. However, some may experience increased thirst, frequent urination, fatigue, and blurred vision.
Q. How is gestational diabetes diagnosed?
A. Gestational diabetes is usually diagnosed through a glucose tolerance test, which involves drinking a sugary solution and having your blood sugar levels tested at intervals.
Q. Can gestational diabetes be managed?
A. Yes, it can often be managed with lifestyle changes like a healthy diet and regular exercise. In some cases, medication or insulin injections may be needed.