Atherosclerosis is a progressive condition characterized by the buildup of plaque in the arteries, which can lead to serious cardiovascular diseases.
Table of Contents
Introduction
Blood vessels including arteries and veins are considered as the basic components of the cardiovascular system. They are not only responsible for the transportation of blood rather they also transport nutrients, oxygen to every cell in the body. In addition, they also facilitate the removal of cellular byproducts and toxic chemicals from the tissue. Any malfunction in the structure of these basic components may lead to many pathological disease states. The most common of which is atherosclerosis. The following article discusses in detail about atherosclerosis including atherosclerosis symptoms, causes, plaque buildup in arteries, risk factors for atherosclerosis, and atherosclerosis treatment options, among others.
What is Atherosclerosis?
Atherosclerosis is a special type of arteriosclerosis where lipid plaques form on the inside walls of arteries. Arteriosclerosis is the hardening of arteries whereas atherosclerosis is a condition in which lipid plaques are formed on the inside walls of arteries and that cause arteries to become narrowed and hardened. Atherosclerosis can be specifically dangerous to the heart as it can affect coronary arteries that are involved in supplying oxygen and nutrients to the heart. In severe cases, blood flow through the coronary arteries is cut off, a heart attack also known as a myocardial infraction (MI) can occur or when heart cells or cardiac myocytes are deprived of oxygen, may die.
Structure of Artery
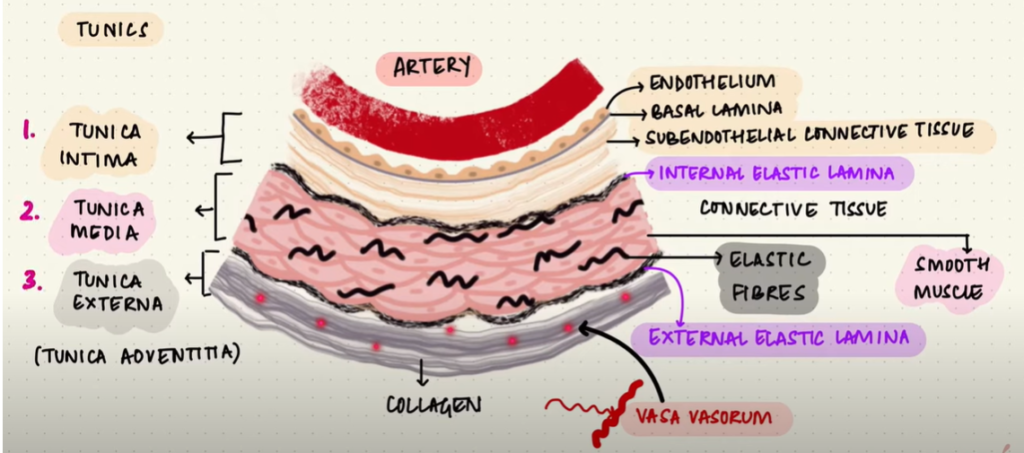
In order to understand the pathophysiology of atherosclerosis, it is important to understand the structure and function of arteries. Arteries are muscular blood vessels. They play a significant role in distributing oxygen, nutrients, and hormones to all parts of the body. They are made up of three layers:
Tunica intima: it is the innermost layer of the artery that surrounds the blood. It is responsible for keeping toxins out of the body, maintains blood pressure and prevents blood clotting. In a nutshell, it maintains smooth blood flow. The innermost cells of the tunica intima are the endothelial cells directly touching the blood flow.
Tunica Media: It is the middle layer of the arterial wall. It is made up of connective tissues including elastic fibres and smooth muscles. This layer is responsible for the smooth flow of blood and expansion and contraction of arteries.
Tunica Externa: It is the outermost layer of the arterial wall. It consists of collagen fibres. This outer layer also consists of nerves and small veins. This layer is mostly responsible for giving blood vessel structure and stability.
Function of Arteries
Arteries carry oxygenated blood (also called as pure blood) and nutrients. The heart pumps oxygen-rich blood into the biggest artery of the body called aorta. This aorta divides into different branches that feed smaller arteries that eventually reach the entire cells of the body. There are different arteries which provide blood to different organs of the body. For example, coronary arteries fetch blood to the heart; carotid arteries fetch blood to brain, head, face and neck. Likewise, there are other arteries responsible for transferring blood to different organs of the body.
Role of LDL in the Blood Vessel
Low-density lipoproteins (made of lipids and proteins) are produced in the liver and then released into the bloodstream. They are responsible for delivering cholesterol to different cells of the body. LDLs transport cholesterol because cholesterol is a vital substance needed by the body for various functions. For instance, cholesterol is an essential component of the cell membrane; it is also required for the synthesis of steroid hormones, bile, and Vitamin D. Since cholesterol is not water-soluble, it cannot travel into the bloodstream freely. LDLs act as carriers that enable cholesterol and other lipids to move through the blood to where they are needed.
Pathophysiology of Plaque buildup in arteries
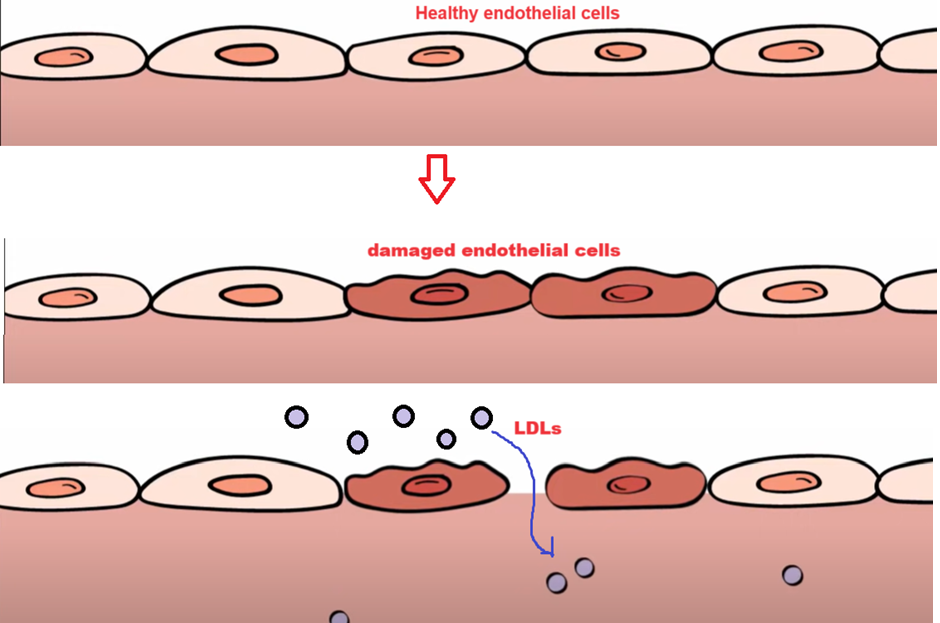
In a normal condition, most of the LDLs pass through the endothelial cells by transcytosis from the blood and enter body cells by receptor-mediated endocytosis to be used in normal cell processes. The progression of atherosclerosis begins when the endothelial cells of the arterial wall become damaged. This can be caused by hypertension, smoking, hyperglycaemia and hypercholesterolemia which is an increased number of LDLs in the blood. Endothelial cell damage increases the permeability of the arterial wall allowing LDLs to enter the Tunica Intima.
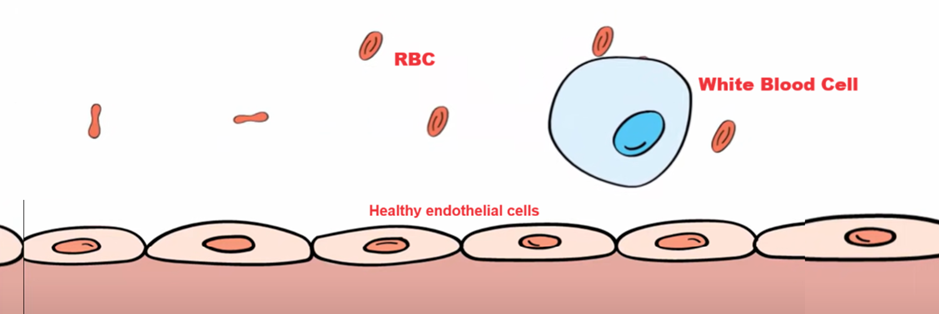
White Blood Cells (WBCs) such as monocytes normally move freely through the blood vessels and do not attach to endothelial cells. However, when endothelial cells are exposed to irritating stimuli or damage, they will express adhesion molecules that can capture nearby WBCs.

The white blood cells undergo morphological changes that allow them to flatten and squeeze between endothelial cells. This movement of white blood cells out of the bloodstream is called diapedesis. White blood cells are capable of producing free radicals and when these free radicals come in contact with LDLs, oxidation occurs. Oxidized LDL particles are especially effective at attracting and activating more white blood cells (macrophages). White blood cells that engulf the modified LDL particles stimulate them to produce even more oxygen free radicals. It becomes easy to imagine that an area of endothelial damage will lead to an accumulation of modified LDL particles and migrating white blood cells inside the Tunica intima.
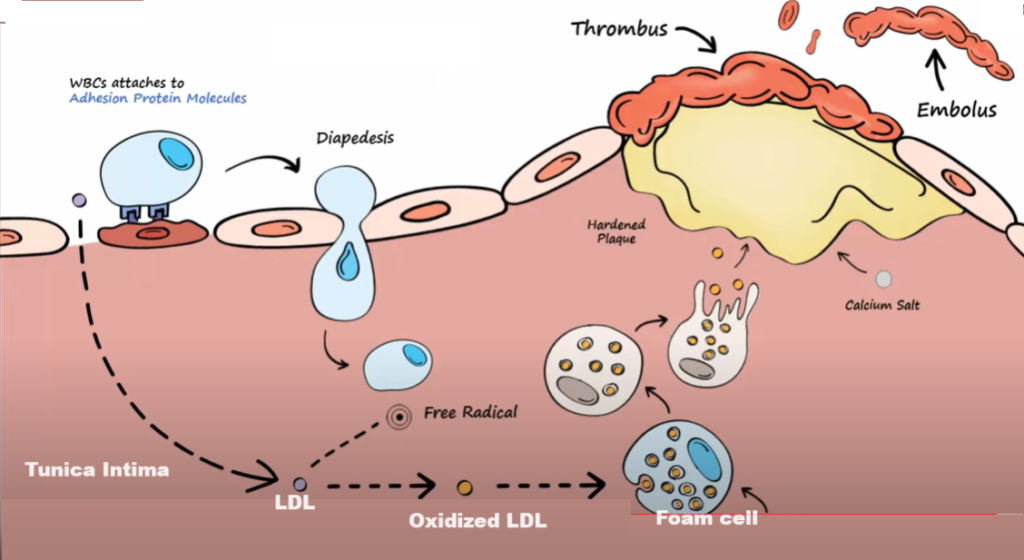
Macrophages in the Tunica Intima start to engulf modified LDL particles. This ultimately leads to the production of a cell called foam cell (lipid-filled macrophage). A foam cell is saturated with LDL particles and the excessive amount of lipid in the cell gives the cytoplasm a foamy appearance. Foam cells ultimately die and release their contents which are quickly engulfed by other nearby white blood cells. Eventually, the accumulating lipid from the processes mentioned above and the fragments of dead cells produce an area with the lipid core that begins to form a plaque.
Endothelial cells cover the plaque. The plaque accumulates calcium salts and more dead cells over time and it will harden. This plaque in the arterial wall is atherosclerosis. If the endothelial cells over the plaque are compromised, blood clots can form on the vessel wall. It is important to note that healthy endothelial cells normally express inhibitors of clotting, but since they are damaged, they no longer do this. Over time, ruptured areas of plaque may create a situation where an area of plaque may jut out into the vessel lumen. A clot that forms and attaches to the wall is called a thrombus. If the clot breaks loose from the arterial wall and floats downstream to even smaller vessels, it is called an embolus.
Atherosclerosis symptoms
In its early stages, atherosclerosis may not present any noticeable symptoms. However, as the condition progresses, individuals may experience:
- Chest pain
- Shortness of breath
- Fatigue
- Pain or heaviness in legs, especially when walking (claudication)
It is crucial to seek medical advice if any of these symptoms occur, as they may indicate significant arterial blockage.
Risk Factors for Atherosclerosis
Atherosclerosis is a condition where the arterial wall becomes hardened and the lumen narrows down over time. Several risk factors contribute to the development and progression of atherosclerosis:
- High Blood Pressure (hypertension)
- High cholesterol levels
- Smoking
- Diabetes
- Obesity
- Lack of physical exercise
- Unhealthy diet
Prevention of artery hardening in atherosclerosis
Preventing artery hardening involves the management of risk factors through lifestyle changes. Some of the prevention methods are mentioned below:
Reduce Saturated and Trans Fats containing Food: It is important to avoid foods rich in saturated and trans fats. In other words, avoid eating fried and processed foods. These fats can raise LDL levels significantly.
Consume fruits and vegetables: Eat more fruits and vegetables. Include whole grains, and legumes in your diet. These sources are rich in antioxidants and fibres that protect against atherosclerosis.
Include Omega-3 Fatty Acids: Include foods rich in omega-3 fatty acids such as salmon fish and mackerel. Dry fruits such as walnuts and flaxseeds rich in omega-3 fatty acids help reduce inflammation and lower blood triglycerides.
Minimize Na Intake: It is important to limit salt consumption. Excess salt consumption leads to high blood pressure and the risk of artery hardening.
Exercise Regularly: Regular physical activity is a must for obtaining good health. Add activities such as brisk walking, cycling, and running in your life. Regular exercise is essential for maintaining a healthy weight. This also lowers blood pressure, improves cholesterol level, and reduce the risk of diabetes.
Weight Management: It is very important to keep the normal body weight. A healthy weight reduces the strain on the heart, lowers LDL cholesterol, and decreases blood pressure, etc.
Quit Smoking: Smoking is one of the main reasons for heart diseases including atherosclerosis. Smoking damages the endothelial layer of the blood vessel, raises LDL cholesterol, promotes blood clot formation and contribute to artery hardening.
Diabetes Management: Blood sugar control is essential to prevent various health diseases. Maintaining a normal blood sugar level is essential for the prevention of atherosclerosis in people with diabetes.
Stress Management: Stress is one of the main reasons for various heart diseases. Chronic stress can increase blood pressure and promotes unhealthy habits such as overeating and smoking. Techniques such a yoga, meditation, deep breathing exercises can help manage stress.
Get Regular Health Check-ups: It is important to undergo regular health checkups to monitor blood pressure, cholesterol levels, and blood sugar level, etc. Health check-ups help in the detection and management of risk factors that can lead to atherosclerosis.
Complications in atherosclerosis
The build-up of plaques in the arterial walls can lead to serious health complications in different body organs. The complications arise as a result of narrowing of arteries, reduced blood flow, and blockage in the artery. Here are some of the key complications of atherosclerosis:
Coronary Artery Disease (CAD): If a plaque in the coronary artery ruptures, a blood clot can form. This leads to the blockage of blood flow to the heart muscles. This can eventually lead to heart attack (Myocardial Infraction). This is a condition that leads to permanent damage to the heart muscle or even death.
Another coronary artery disease is angina (chest pain). Angina is the result of reduced blood flow to the heart due to narrowed coronary artery.
Carotid Artery Disease: Atherosclerosis in the carotid arteries can lead to stroke. Carotid arteries supply blood to the brain. A stroke occurs when a blood clot blocks blood flow to part of the brain. This can result in brain damage, disability, or death.
Peripheral Artery Disease (PAD): Atherosclerosis in the arteries of legs or arms can lead to peripheral artery disease. It reduces the blood flow to the limbs. PAD can cause pain, cramping or weakness in legs during physical activities, also known as claudication.
Chronic Kidney Disease: Renal artery stenosis occurs due to atherosclerosis. In this condition, due to narrowing of arteries, blood supply to the kidneys is reduced significantly. I
Prevention of Atherosclerosis
Lifestyle changes are required to treat atherosclerosis. Lifestyle changes can significantly help keep the arteries healthy. Some of the prevention methods include:
- Quit smoking
- Regular exercise
- Eat healthy foods
- Maintain a healthy body weight
- Maintain a healthy blood pressure
- Check cholesterol levels and blood sugar levels
Diagnosis and Treatment of Atherosclerosis
Diagnosis of atherosclerosis not only involves physical examination, it also involves medical history, blood tests, and imaging studies. The following are the key diagnostic tests required to confirm the presence and extent of atherosclerosis.
Medical History: The health professional will look for risk factors such as high blood pressure, high cholesterol, diabetes, and family history of heart disease.
Physical examination: During physical examination, the health professional may listen for abnormal sounds in the arteries using a stethoscope. The health professional will also look for blood pressure in different limbs and examine signs of poor circulation, etc.
Blood tests: Several blood tests are done such as lipid profile (to measure levels of total cholesterol including LDL and HDL).
Blood Sugar: A fasting blood sugar test or HbA1c is done to detect diabetes. Diabetes is one of the significant risk factors for atherosclerosis.
Inflammatory Markers: Tests like C-receptive protein (CRP) may be used to detect inflammation in the body.
ECG or EKG: Records of electrical activity of the heart are used to detect signs of previous heart attacks, abnormal heart rhythms, or reduced blood flow to the heart muscle.
Imaging studies: There are several imaging studies required to confirm atherosclerosis. Some of the imaging studies include carotid ultrasound, abdominal ultrasound, Ankle-brachial Index (ABI), CT scan, CT angiography, magnetic resonance angiography (MRA), angiography, and other specialized tests such as electrocardiogram, and PET scan tests are done.
Treatment of Atherosclerosis
Lifestyle changes play a significant role to treat atherosclerosis. However, in severe cases, medication or surgical procedures may require. Medications are given by the health professional depending on the severity of atherosclerosis. On the other hand, surgical procedures may include angioplasty and stent placement, endarterectomy, fibrinolytic therapy, and coronary artery bypass graft surgery, to name a few.
Conclusion
Atherosclerosis is a serious cardiovascular condition caused by plaque buildup in the arteries. This can lead to complications like coronary artery disease, stroke, and peripheral artery disease. It’s important to understand its causes, risk factors, and the need for lifestyle changes to prevent it. Early detection through tests can help manage the condition. Treatment options include lifestyle changes, medications, and surgery. Regular check-ups, a healthy diet, exercise, and quitting smoking are essential to prevent atherosclerosis and maintain heart health.